6 minutes
The tilt table is a test performed to determine possible causes of symptoms such as dizziness and syncope. Read on and learn what the procedure is like and when it is recommended.
The tilt table test, also known as inclined table, used to help determine the source of various symptoms that have no apparent cause. These include syncope, dizziness, feeling unsteady, and sudden sweating..
As the name implies, the tilted position of the body is varied during the tilt table test. In this way, they try to appreciate the changes in blood pressure and heart rate.
Medicine may be given in some cases. And although in general it is a fairly simple and non-invasive procedure, there are contraindications.
What is the tilt table test and what is it for?
When we are standing, the force of gravity causes the blood to flow more towards the lower part of the body. But to counteract this effect, the circulatory system makes certain adjustments automatically.
This setting consists of a slight increase in heart rate and a vasoconstriction on the legs, thanks to which blood and oxygen continue to flow to the brain. This is how we can stand for a long time.
Although in certain cases the system may not work properly. This results in a drop in blood pressure and heart rate. (bradycardia), with the consequent manifestation of various symptoms.
The tilt table test is performed to induce the conditions in which such symptoms occur.. In this way, it helps diagnose the possible cause of dizziness and fainting when there are no other apparent reasons.
When is the tilt table test recommended?
The tilt table test can be performed in young, apparently healthy patients, as well as older adults. Recommended when a diagnosis has not been made with other tests, such as EKG, brain MRI, or angiography.
In particular, it applies if a condition is suspected or certain symptoms are present:
- Postural orthostatic tachycardia syndrome.
- Neural-mediated syncope.
- Vasovagal syncope.
- Orthostatic hypotension.
- Ventricular cardiomyopathy.
- Sudden loss of consciousness
- Jerky involuntary movements.
- Frequent falls with no apparent cause.
- Feeling of light-headedness.
- Palpitations associated with changes in position.
- Slow or irregular heart rate
Tilt Table Test Preparation
When a tilt table test is scheduled, the doctor should be consulted regarding the preparation and the precautions that must be taken beforehand. In relation to this, the following recommendations are suggested:
- Medicines: You may need to stop taking drugs that affect your heart rate or blood pressure one day before the test.
- Feeding: The night before you can eat as normal, but nothing should be eaten 4 hours before the test.
- Clothing: comfortable clothing and shoes should be worn.
- Companions: It is recommended to be accompanied on the day of the test, in case someone else is required to drive you home.
- Allergies: You must inform your doctor if you suffer from any allergies.
How is it the procedure?
The tilt table test is a simple, non-invasive outpatient procedure. It can be done in a hospital or office setting.
To begin the test, the patient has to remove jewelry, clothing, watches, or other objects. You should also undress from the waist up and put on a gown.
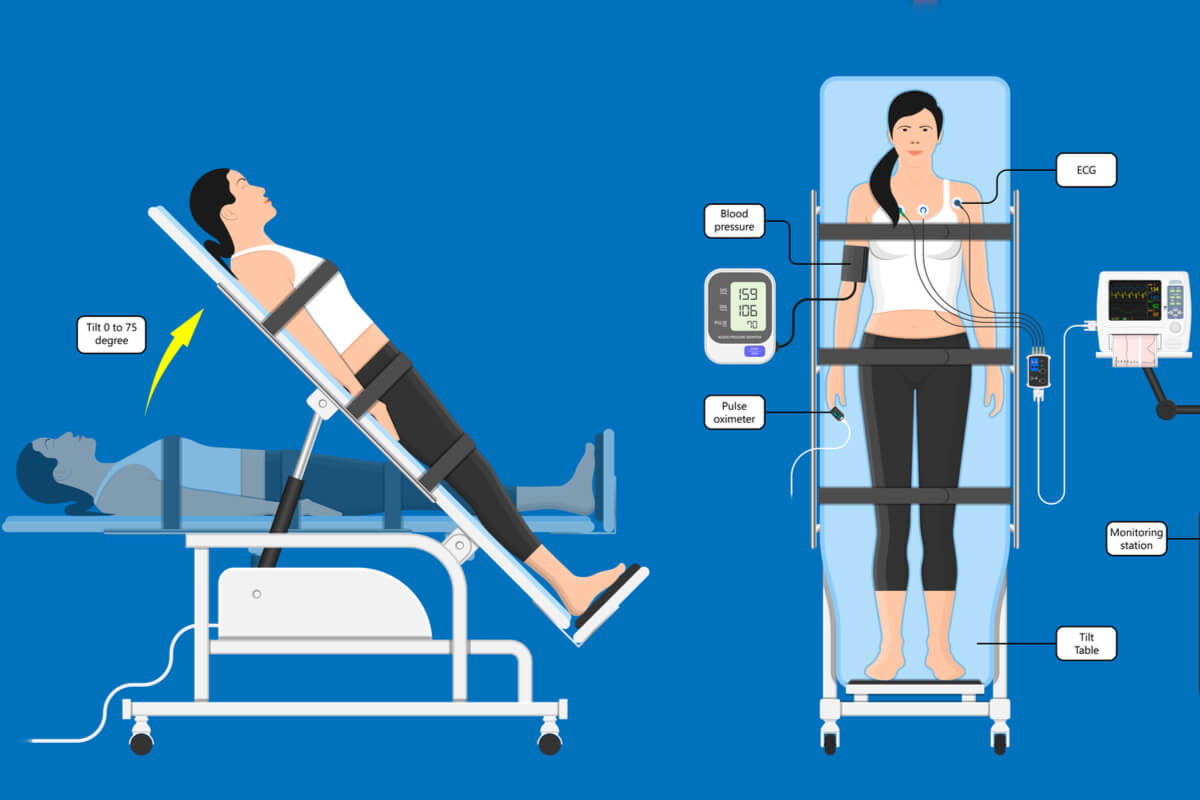
Then the person lies on the tilt table. The doctor will adjust the strap straps around the patient’s body.
At once, adhesive patches are attached with electrodes in different areas (chest, legs and arms). These are connected to an electrocardiograph, with which the heart rate is monitored.
In addition, a blood pressure monitor is used. A line is also placed in one of the veins in your arm to give medications intravenously if needed.
First signs are assessed while the person is lying down, in a completely horizontal position. Then the table tilts, raising the head 30 degrees and then 60 degrees; thus, until the person is vertical.
Blood pressure, heartbeat and oxygen levels will be measured at all times. In some cases, a drug, such as isoproterenol or nitroglycerin, may be given to induce changes in the heart rhythm.
The procedure usually takes about an hour. After the tilt table test is complete, the sensors and straps are removed.
What do the results mean?
If the values are altered, the test is positive. On the contrary, if the person does not react to changes in position on the tilt table, it is considered negative. In general, altered blood pressure denotes orthostatic hypotension, and a decreased heart rate would indicate vasovagal syncope.
However, a negative result does not rule out the possibility of a condition. It just means that the test doesn’t reveal it. According to studies, there is a false positive rate that can be between 5% and 20%.
Additional tests may need to be done. For example, the use of a Holter monitor or other procedures, such as hemodynamic testing with ultrasound or echocardiography, may be suggested.
Possible risks and contraindications
The tilt table test is generally safe.Although not common, complications include nausea, vomiting, fainting, weakness, low blood pressure, headache, and palpitations.
If vital signs change drastically or if the person does not feel well during the procedure, the test can be stopped. Some treatment may be required to stabilize the patient.
If the discomfort persists in the next 24 hours it is recommended to rest. But beyond this time, it is advisable to call the doctor. The same should be done if there are vision changes, chest pain, or seizures.
A tilt table test is not recommended if the person has certain conditions:
- Very low blood pressure
- Ischemic heart disease
- Diabetes mellitus.
- Glaucoma.
- Prostatic hypertrophy.
- Severe valve disease.
- Hypertrophic cardiomyopathy.
Diagnoses and treatments to be instituted
Most people experience slight drops in blood pressure and slight elevation of heart rate when standing up, whether they have been sitting or lying down. Although the speed and degree with which these changes occur and their association with other symptoms can be decisive.
Hence that the tilt table test alone is considered not to provide a definitive diagnosis. For this reason, the doctor must evaluate the results taking into account the entire clinical history of the patient; even considering other evidence before making a decision or recommending treatment.
If the results point to orthostatic hypotension, medications will be recommended to raise or prevent drops in blood pressure. For its part, vasovagal syncope is slightly more difficult to treat, although there is the possibility that medications may also be recommended.